Today I spoke at the Palliative and Hospice Division at NorthShore University Health System Symposium, Living With Dementia: Best Practices for High-Quality Palliative Care, which took place at the Chicago Botanic Garden.
The course objectives included: 1) Discuss the challenges our systems face in the care of patients with severe dementia. 2) Illustrate the psychosocial challenges families and caregivers encounter when living with people with dementia. 3) Design supportive programs to improve the quality of care of the end of life in patients with dementia.
Theresa Dewey; Manager of Care Navigation and Early State Engagement, Alzheimer's Associate of Greater Illinois; and I co-presented. I was listed as "Former caregiver and advocate for families of Alzheimer's patients."
Here is the text of my presentation:
DEMENTIA & ON-GOING GRIEF
A Presentation by Michael A. Horvich
The Palliative and Hospice Division at
NorthShore University Health System
September 30, 2016
SLIDE: TITLE
SLIDE: DISCLOSURE
SLIDE: NAMASTE
The story I am about to share with you is very personal. I’m comfortable with crying in front of you, however it is very difficult to cry … and speak at the same time.
So if I do get choked up, I will pause, take a few deep breaths, and be right back. Thank you for your understanding.
PART ONE: BACKGROUND
The story I will share with you today has been divided into eight parts, each announced by a screen like this.
• • • • •
I am NOT presenting this story to you today as an EXPERT in the field of GRIEF … NOR as an EXPERT in the field of DEMENTIA/ALZHEIMER’s … but rather as someone with the DIRECT EXPERIENCE of having LIVED through BOTH of these situations.
Gregory … my same sex partner, my husband of over 41 years … and I … lived for 12 years with the diagnosis of Dementia, most likely Young Onset Alzheimer’s Disease.
I might add that we lived WELL, refusing to accept the diagnosis as a “death sentence. Also, I never referred to it as HIS diagnosis but rather OUR diagnosis.
I used to tell people that on a SCALE OF DIFFICULTY … from TERRIBLE to TERRIBLE … living with DEMENTIA was HORRIBLE.
GREGORY, for the most part dealt with HIS GRIEF in his usual CALM manner and the Alzheimer’s created a BUFFER which kept him from being fully aware of the changes through which he was going.
PART 2: MEDICALIZATION
We were RELIEVED when we received the diagnosis because now we had an idea of what we were dealing with … although at the time we did not REALLY understand the nature of the roller coaster ride we would be on for the next 12 years.
Being an incurable, progressive illness what could our doctors really do during those early stages except confirm my existing observations?
I knew that what Gregory and I were experiencing was due to a MEDICAL CONDITION and the changes taking place in his brain were affecting all parts of his existence.
But that was all the time I devoted to the MEDICAL aspects of our experience.
The MEDICAL ASPECTS were not able to provide any PEACE OF MIND and little SUPPORT during the our journey with DEMENTIA.
I read and educated myself on the types, causes, and trajectory of the disease, often putting down the material because I did not really want to know what would be coming in the future.
At the END of Gregory’s life … our doctors and the medical profession provided GREAT support.
PART 3: CAREGIVING PARTNERS
In the beginning I REFUSED to refer to myself as Gregory’s CAREGIVER. I did what I did because I LOVED him. I saw caregivers as his doctors, nurses, health aids, etc.
I refused the LABEL out of RESPECT for not wanting to diminish Gregory, my life partner, to the role of my “PATIENT.”
He was the MAN I loved BEFORE the diagnosis and continued to be the MAN I loved after the diagnosis!
We had been a TEAM for so many years and my attitude was to keep it that way even though over time Gregory’s ROLE on the team changed.
EVENTUALLY, Gregory’s cognitive and self help abilities were so diminished, that REALITY FORCED me to consider myself a Caregiver.
PART 4: A NEW SENSE OF FAMILY AND HOME
Rather than thinking about the Dementia in terms of its MEDICAL implications, I worked very hard at CREATING A NEW SENSE OF FAMILY and HOME for Gregory and me.
We modified our life, our home, and our relationship … to fit Gregory’s changing needs.
I learned bit by bit … how to lower expectations for him as Gregory’s abilities changed and how to more simply communicate with him.
Sometimes the modifications became an ongoing event, with my having to become more and more creative in helping to provide for and nurture Gregory in all ways environmental, safety, physical, medical, mental, emotional, and social.
MY GRIEF over time regarding HIS losses in addition to what I was loosing, were beginning to take its toll … but rather than wallowing in our situation … I actively worked at making our life and days as normal and enjoyable as possible … and that helped me to cope with the situation.
Our love continued to grow each day. Gregory felt safe, protected, supported, loved, and contented. He was able to enjoy his life.
His feeling this made me feel that what I was doing was successful.
With all the changes, he was still my partner, soul mate, best friend … but it and he were different. I felt so very alone.
PART 5: LIVING WITH DEMENTIA 365/24/7
As Gregory’s Dementia / Alzheimer’s progressed, I remember thinking many times, “If the disease would only stop progressing at this point, I would be content.”
But progress it did … and the RESTING, level periods were shorter AND the need to re-think and re-establish NORMALCY in FAMILY and HOME continued, sometimes on a daily basis.
Often, Gregory’s behavior or perceptions were what I only could call … CRAZY.
Sometimes the situation was so confused and disoriented that I not only didn’t know how to SUPPORT Gregory … but I didn’t know how to INTERPRET what he or I were experiencing.
His abilities would unexpectedly come and go, they would return … but at a weaker level, then they would disappear only to appear again at a later date and sometimes or eventually never to be seen again.
Being able to monitor and provide for Gregory’s needs in a RESPECTFUL way was increasingly more difficult. But I didn’t give up!
Not making assumptions or lowering expectations before they needed to be and at the SAME time not creating unnecessary stress and frustration on Gregoryo’s part … was more and more a guessing game.
SLIDE: GRIEF
My bouts with MILD DEPRESSION and GRIEF increased.
Early on I had turned to my computer to write and to process my experiences, since I could no longer talk these things through with Gregory.
I learned to cry myself to sleep at night without shaking the bed so I would not wake him.
Sometimes he and I would have a cathartic cry together … or a MEAN exchange followed quickly by apology … but for the most part, I dealt with my grief alone.
Many long term “friends” deserted us. I understood their not being able to witness the changes Gregory was going through but none-the-less, their desertion HURT! And I was SAD and ANGRY.
• • •
Now and then I would arrange a “playdate” for Gregory with a good friend. This allowed me time to myself and Gregory had a good time as well.
As he needed more and more support and when he could no longer be alone, I hired Northwestern University students to spend time with him, a couple times a week.
About four or five years into our journey, I was fortunate to find, Peter, my Jungian Psychologist who really met my needs.
He supported me when I was on target with my thinking and challenged me when I was off.
I read about and learned how to meditate. Both Gregory and I had studied various Buddhist teachings and felt comfortable with them.
I met Corinne … I call her my Guru … and she helped me continue on my path to understanding meditation, Yoga Nidra, and Buddha’s teachings.
To this day, I attribute my studies in Buddhism in helping to keep me sane and to support me through our journey with ALZHEIMER’S in ways that my Judaism and Gregory’s Catholicism could not.
It gave me hope … at least on a day to day basis … that our life could be OK.
PART 6: MEMORY CARE FACILITY
Gregory was able to be at home with me for most of his twelve years with DEMENTIA.
By year 10 and a half, his medical and physical needs became so great, that short of turning the condo into a fully staffed 24/7 hospital ward, I was not able to provide for his needs.
Gregory moved to the Lieberman Center for Health and Rehabilitation, in Skokie, where I now had an on-duty team of medical and support people to help me with anything that might come up.
At first I felt guilt moving him to Lieberman … you know that “promise me you’ll never put me in a home” plea by a loved one. Gregory, on the other hand never once asked to go home or questioned why he was at Lieberman.
Quickly I realized that Gregory’s new sense of community and belonging, the safe clean environment, the delicious meals, and the presence of many people around him were all positive attributes of my decision and contributed to his well being.
I visited him every day. Our time together was quality time … with Lieberman picking up the DIFFICULT support needs.
Now and then he would become frustrated or angry … but he did not complain much and was usually kind and compassionate with me, himself, and others.
The staff and administration at Lieberman were supportive and available to Gregory and me whenever needed when it came to MEDICAL issues.
SLIDE: SOCIAL/EMOTIONAL
Lieberman did NOT do as well with SOCIAL/EMOTIONAL issues, which I believe might be MOST important thing one can do for DEMENTIA residents.
The activities department, art therapy, special programs, concerts, and holiday events etc, HELPED … but days can be VERY LONG, LONELY, and ISOLATING for a person with DEMENTIA.
NURSES time is taken up with medical issues.
Most of a Certified Nurse Associates’ time is spent on cleaning up residents when soiled, hygiene and bathing needs, transporting residents from place to place, and helping with feeding.
There is very little time left for one on one SOCIAL/EMOTIONAL engagement or even time to facilitate it between residents who are still able to do so.
To provide for the SOCIAL/EMOTIONAL aspects of Gregory’s life, I was FORTUNATE in finding and being able to AFFORD, MANNY, a PRIVATE PAY, DAY CARE HELPER, who was with Gregory seven days a week from 11:00 AM until 6:00 PM.
All things considered, we were very fortunate to have found Lieberman and I continue to be grateful for our 18 months there. I would highly recommend the facility to anyone who asked.
Due to two hospitalizations early in his stay at Lieberman; including a fall with head injuries, a grand mal seizure, and catching the flu … his condition worsened.
Gregory, who had been ambulatory until then, even with support from Physical and Occupational Therapy, was now confined to a wheelchair.
At times it was difficult making important decisions about Gregory’s health without his input, which by now he was not able to give, and I had to talk myself through not feeling guilty in making these decisions on his behalf.
I would always explain these changes to him but never knew whether he really understood me or not.
With Lieberman and Manny’s support my life calmed down quite a bit … but when Gregory was ill, his meds needed re-evaluation, or we would encounter care difficulties; or when I was ill; life would again feel like being on a roller coaster.
It always continued to feel sad.
PART 7: HOSPICE
Midwest Hospice, now Journey Care, joined our team and worked hand in hand with The Lieberman Center for the last 9 months of Gregory’s life.
I am SO GRATEFUL to the hospice nurses, social workers, aides, doctors and to the CONCEPT of hospice itself.
Without their help, our journey and Gregory’s eventual death would not have been as smooth and peaceful as it was and they helped me to understand and educate myself on the process of living … and dying … with DEMENTIA.
Towards the middle of Gregory’s stay at Lieberman; he became very agitated, somewhat aggressive, depressed, unhappy, and much more frustrated than usual.
Some of you may not like to hear me say this … but after careful study and deliberation; the nursing staff, Gregory’s doctors, Hospice, and I decided to put him on Risperdal, an anti-psychotic drug.
The dosage was VERY carefully monitored and the end results were that Gregory began to enjoy his life again and the quality of his life increased. Using Risperdal worked for US, it might not work for everyone and should be used only with extreme careful consideration and monitoring!
I know that antipsychotic drugs often get a bad rap when used in nursing facilities, but in our case, I believe they were used very carefully and in GREGORY’S BEST INTERESTS … not in my interests or those of the facility or staff as the bad rap often implies.
Also I understand that with older people, the chance of heart attack and death might be higher, but I look at the alternatives and say it is a risk worth taking.
• • • • •
Gregory and I had talked about END OF LIFE PLANS while he was still able to do so. We decided, “ DO NOT RESUSCITATE” and “NO HEROICS.” If we are dying, just keep us comfortable and hold our hand.
By extrapolation, after long conversations with Hospice, I decided that in the event of Gregory’s coming down with a bad cold moving towards Pneumonia, we would NOT administer antibiotics.
I did not want to do anything that would INADVERTENTLY prolong his life since I knew it would only get worse and worse.
All decisions of this nature were made with what was best for Gregory in mind and made with love. I know that Gregory would have agreed with my decisions.
PART 8: GRIEF
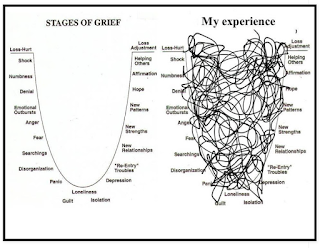
For this presentation, I needed to make clear in MY mind … ways of thinking about GRIEF.
Theresa discussed some of the clinical aspects of GRIEF, but let me show you just briefly what I thought about.
SLIDE: HEALTHY vs UNHEALTHY
This is probably the most obvious. All types of GRIEF, while causing various degrees of suffering and pain and duration, can be experienced in a HEALTHY way or in an UNHEALTHY way.
I cannot say why one person deals with GRIEF in one way and another does it in another way … other than to reflect on how each person approaches life in their own unique way.
SLIDE: GRIEF DIFFERENTIATION
To clarify my thinking further, I have COMBINED — ANTICIPATORY and ONGOING GRIEF — into what I call —COMPLEX GRIEF.
ONGOING GRIEF continues over years, while ANTICIPATORY GRIEF ACTIVELY HIDES in the background and is additive … as one anticipates loss after loss, change after change … and anticipating the eventual arrival of DEATH.
COMPLEX GRIEF makes dealing with GRIEF while coping with DEMENTIA/ALZHEIMER’S much, much more difficult.
Finally, the GRIEF which arrives with the DEATH of a loved one, I have labeled END POINT GRIEF.
I do not mean that GRIEVING for the loved one ever really ENDS, just that the ALZHEIMER’S has ENDED and DEATH has arrived.
• • •
ALL GRIEF affects a person PHYSICALLY as well as EMOTIONALLY. COMPLEX GRIEF … MAGNIFIES the effects.
EMOTIONALLY the person deals with among others: increased irritability, numbness, bitterness, detachment, frustration, preoccupation with loss, and inability to show or experience joy.
… I have experienced ALL of these!
PHYSICALLY the caregiver deals with among others: appetite and digestive problems, fatigue, headaches, chest pain, back pain, sore muscles, illness, difficulty breathing, and difficulty sleeping.
… I have experienced ALL of these!
These EMOTIONAL and PHYSICAL symptoms can wreak havoc when experienced on a MULTI YEAR / 365 day a year / 24 hours a day / 7 days a week basis.
SLIDE: GREGORY & MICHAEL
COMPLEX GRIEF takes a MAGNIFIED toll on the caregiving partner causing inappropriate or angry reactions to the symptoms of DEMENTIA, depression, allowing for neglecting one’s health, turning to comfort eating which usually becomes unhealthy eating, use of alcohol or drugs, fosters illness … and can cause early death of the caregiver.
• • • • •
At times I wished for GREGORY’S death … partly so he would no longer have to deal with the continued frustration, confusion, diminishing of his abilities and scope of life … but also to allow me to move on with my own life. Of course, this made me feel guilty.
IN LOOKING BACK, however, sharing those 12 years of DEMENTIA with Gregory were VERY IMPORTANT to me AND to him and I am grateful for having had them.
Over time, learning to sit with, experience, understand, look for lessons in, and accept … GRIEF … helped me to ride GRIEF out.
My continued studies in Buddhism, working with my therapist and my Guru, doing what I could to keep Gregory happy and safe, taking short 3 or 4 day vacations, reclaiming my life as I best could with support from family and friends … all helped with the GRIEF.
I always RESENTED when people would tell me that I needed to “TAKE CARE OF MYSELF.” I was doing the best I could …but loving someone with DEMENTIA/ ALZHEIMER’S is no easy task.
And unless you are in the middle of it yourself, you cannot really know what it feels like.
While my COMPLEX GRIEF continued strong, over time it was more tolerable and less debilitating.
• • • • •
SLIDE: END POINT GRIEF
Last October, due to complications of end stage Dementia and Pneumonia, Gregory took three days to prepare himself to die.
With the help of Hospice and the Lieberman staff, he passed peacefully and with the help of Hospice, it was easier for ME to live through and accept his dying.
When he died, I said my goodbyes and left his body to Hospice for final handling. I stopped when I reached my car to analyze what I was feeling.
Besides amazing sorrow, I felt JOY at Gregory’s having moved on to his next adventure, JOY at MY being able to move on with my life, and FREEDOM.
And I had the insight that at the MOMENT Gregory left his physical body … the Alzheimer’s DISAPPEARED. POOF, went up in smoke, gone!
ALL the difficulties of Alzheimer’s for both Gregory and me: the confusion, the frustration, the anger, the fear, the losses, the pain, the sorrow, the GRIEF; had disappeared and Gregory was O K again! … And so was I!
OR SO I THOUGHT …
SLIDE: NEVER REALLY KNEW
I had not yet begun my END POINT GRIEVING over Gregory’s death and never really UNDERSTOOD the FULL nature of GRIEF until Gregory died. I WASN’T READY when it hit!
I cried, I howled, I learned a new word: KEENING. I felt ill, I didn’t sleep or eat well, I just felt numb. I felt guilty, I felt angry.
Often I felt on the verge of panic and felt that if I gave in fully to my emotions, I would have to be sedated and possibly would never come back to myself.
In looking back, the COMPLEX GRIEF was DIFFICULT … but it was NOTHING compared to the END POINT GRIEF which arrived when Gregory died.
Before there was always hope, there was always tomorrow, but now the FINALITY of death … and the loss of Gregory’s and my PHYSICAL relationship, began a new era for me.
• • • • •
Over time, I have worked at establishing new ways of having a physical relationship with Gregory.
SLIDE: SHRINE, PHOTO, BEARS
I set up a shrine for him on the bookcase in my bedroom.
A framed photograph of us shortly before he died sits on my desk.
I carry a small amulet, a bronze teddy bear, filled with a small bit of his cremains, in my pocket … and I carry him with me in my heart and mind as well.
Besides the legacies of the love that Gregory shared with me and so many others, there are two legacies for Gregory which have also helped with my GRIEF.
The DOCUMENTARY, which you watched earlier, has been accepted by 50 film festivals so far, locally and around the world, and has won 22 awards.
Hundreds of thousands of people, including you now, have shared Gregory’s and my love story.
The second legacy is the creation of the MORE THAN EVER EDUCATION FUND, in Gregory’s memory, which will provide college scholarships to Chicago Area youth confronting homelessness and will be administered by the premier Chicago not-for-profit, La Casa Norte.
• • • • •
I begin to realize a NORMALCY in the process of GRIEVING … its unique character and pain … the inability to “CONTROL” it … and by the BELIEF … and HOPE … that “IT DOES GET BETTER OVER TIME!”
SLIDE: GREAT LOVE/ GREAT GRIEF
I learned to ignore OTHER’S ideas about HOW and HOW LONG I should GRIEVE … which is advice you should never offer to a person who is grieving … unless asked for … or deemed medically, destructively, unhealthy!
I learned to accept that the PAIN of DEEP GRIEF is the COST for GREAT LOVE!
SLIDE: A YEAR AGO
Now, almost a year after Gregory’s death, in my nightly conversations with him, I end saying, “It was a GOOD day!” … and you know what, my days HAVE BEEN good.
By now I feel comfortable in my GRIEF … even when it returns periodically, unexpectedly, or stronger than usual.
I attribute some of this to the fact that for MORE than twelve years now; I have been processing his illness, the changes in our relationship, and Gregory’s eventual death.
So in some ways, COMPLEX GRIEF, while it takes its magnified toll, when dealt with in a HEALTHY way, can help prepare for the arrival of and getting on in healthy way with END POINT GRIEF.
• • • • •
In my story I have tried to share with you some of the ways in which I have dealt with the COMPLEX GRIEF which came over time with Gregory’s DEMENTIA/ALZHEIMER’S as well as the END POINT GRIEF which arrived with Gregory’s death.
SLIDE: GREGORY
How did I survive the ordeal?
First, I believe that GREGORY’S and MY GREAT LOVE for each other and our LONG TERM HEALTHY, RESPECTFUL RELATIONSHIP made the difference.
Secondly, by actively working to make Gregory’s life as safe, comfortable, peaceful, engaging, and loving as possible …
… by taking care of myself when I could
… by avoiding the MEDICALIZATION of our experience and rather spending time and energies CREATING A NEW SENSE OF FAMILY and HOME
… the GRIEF was more tolerable.
SLIDE: COPING
Finally, the points as shown in this summary of what I have shared with you during this presentation, have ALL contributed, I believe, to my ability to GRIEVE in an ACTIVE, HEALTHY, SUCCESSFUL way.
• • •
This brings my presentation to a close. If you would like a copy of my Power Point or for a full text of my presentation, my bibliography in your handout explains how you can accomplish that.
At this point in our presentation, Theresa and I would be happy to address any questions you may have. Thank you.
END SLIDE: DANDELION























AWESOME presentation!!! The only one small bit that I would take issue with is "I know that antipsychotic drugs often get a bad rap when used in nursing facilities." I understand the small doses of risperdal worked for Gregory and you. However, antipsychotic medications are getting a "bad rap" for a reason. While they may be appropriate for a very small percentage of people (like Gregory) who live with certain kinds of dementia, they are grossly and inappropriately overprescribed to large numbers of people in LTC to sedate them into compliance for the convenience of overburdened staff. The proof of the benefits of reducing the use of antipsychotics continues to grow (e.g. http://myalzheimersstory.com/2016/08/04/what-happens-when-care-homes-stop-giving-antipsychotics-to-elderly-people-with-dementia/)
ReplyDeleteCongratulations on an amazing presentation which I'm sure the audience found both interesting and compelling <3
Thanks Susan for your kind comments. You and I have always had our differences over the use of antipsychotic drugs. I know the research and still feel that the story is not YING and YANG. I did say that in our situation, the drug worked. Best to you.
Delete